Chasing Cheaper Cancer Drugs
In a nondescript suburb south of London, tucked away behind a big hospital, Paul Workman and fellow scientists are celebrating victory in the "World Cup" of cancer drug research for their work in discovering a stream of new medicines.
But the win is bitter-sweet. One of the new drugs behind the coveted prize from the American Association for Cancer Research (AACR) has been deemed too costly to use in state-run British hospitals like the one next door.
It is a stark example of the pricing crisis now facing cancer medicines across the globe.
In developed and developing countries alike, patients and governments are struggling to pay for modern drugs that are revolutionising cancer care but may cost tens of thousands of dollars a year for each patient.
"It's very frustrating," says Workman, who heads up the drug discovery unit at the Institute of Cancer Research (ICR), which is funded in large part by charities.
What is needed, he believes, is a new model that takes advantage of the highly specific nature of modern targeted therapies to slash drug development timelines and costs.
In the long term, Workman is convinced that will happen. But for the moment the world is caught in a pinch point as global drug companies put sky-high price tags on cancer medicines in a bid to recoup development costs for drugs aimed at a relatively small number of cancer sufferers.
The strains are growing - whether in Europe, where austerity has savaged healthcare budgets, or in the United States, where out-of-pocket costs can bankrupt patients, or in the developing world, where price tags of around $5,000 for a month's drug supply are simply out of reach.
India loses patience
India, a country with a long history of making cheap off-patent drugs and a sometimes brittle relationship with Western drugmakers, has finally lost patience.
New Delhi shocked the global drugs industry in March by effectively ending Bayer's monopoly on kidney and liver cancer drug Nexavar and issuing its first-ever compulsory licence, allowing local generic firm Natco Pharma to produce and sell the drug cheaply in India.
In a move to head off the same threat to its patented drugs, Roche, the world's biggest maker of cancer medicines, plans to offer significantly cheaper locally branded versions of two other cancer treatments, Herceptin and MabThera, under an alliance with Emcure Pharmaceuticals.
Further showdowns with Big Pharma seem inevitable. Novartis , for example, is challenging a decision not to grant a patent for its leukaemia drug Glivec in a case that will go to the Indian Supreme Court on July 10.
Michelle Childs, head of policy at Medecins Sans Frontieres and a critic of many industry practices, says the approach taken by Big Pharma to date of excluding the vast majority of people living in developing countries - barring a small but growing middle class - is not sustainable.
She expects powerful countries like India and China, both of which have capacity to make cheap generic drugs, to flex their muscles more in future as the battle over access to medicines enters a new phase.
"Traditionally, the focus has been on drugs for infectious diseases like HIV and tuberculosis, but increasingly developing countries are facing a double burden of disease as we see the rise of chronic diseases like cancer and diabetes," she says.
The issue is not confined to poorer countries - as Workman at the ICR knows all too well.
His team spent many years working on a novel prostate cancer pill that won special recognition in the citation for the AACR prize awarded in Chicago on Sunday (April 1), only to find that Britain's National Institute for Health and Clinical Excellence (NICE) considers it too costly to be used.
If the cost-effectiveness watchdog does not change its mind, Zytiga, which is marketed by Johnson & Johnson and costs 2,930 pounds ($4,700) for a month's supply, will be off-limits for Britons on standard state healthcare.
Significantly, NICE also thinks Bayer's Nexavar is too expensive - highlighting the common concerns about costs shared by healthcare authorities in different parts of the globe.
Such tough calls are inevitable when budgets are limited, according to NICE chairman Mike Rawlins, who says it is time to challenge drug companies about the high prices they seek for products that sometimes offer only modest benefits.
$85 billion sales by 2016
The debate over how to price cancer medicines matters intensely for the pharmaceuticals industry and society at large.
Cancer is a leading cause of death worldwide, accounting for 7.6 million deaths in 2008 and predicted to top 13 million in 2030, according to the World Health Organisation. Some 70% of deaths occur in low- and middle-income countries.
For drugmakers, the disease is a rich seam of sales and profits. Cancer medicines overtook cholesterol fighters as the biggest-selling prescription drug class five years ago and sales are set to hit $85 billion in 2016, up from $58 billion last year and a mere $8 billion in 2000, according to consensus forecasts compiled by Thomson Reuters Pharma.
Cancer is particularly attractive commercially as patents expire and profits wane on drugs in other areas.
Privately, though, even some drug company executives wonder if the industry will be charging such high prices in a few years time.
The price tags on a flurry of new entrants have certainly pushed the envelope, with Bristol-Myers Squibb's melanoma treatment Yervoy costing $120,000 for a four-infusion course and Dendreon's Provenge for prostate cancer priced at $93,000 for a three-dose course.
In the United States, some cancer patients have abandoned medical care because of their bills or else face a significant risk of bankruptcy, according to studies presented at the American Society of Clinical Oncology last year.
Europe's more socialised healthcare system creates different strains. Cash-strapped governments have slashed drug prices, racked up close to $20 billion in unpaid bills for treatments and, crucially, are becoming increasingly reluctant to pay for innovative new drugs.
Andrew Witty, chief executive of GlaxoSmithKline, says European governments are making a false economy by delaying the introduction and reimbursement of promising new treatments, especially for cancer, in their short-term drive to save money.
Pfizer CEO Ian Read told Reuters last month there was a serious "disconnect" between the marketplace in Europe and the desire of governments to sustain a vibrant research base. "Europe is not paying its fair share of innovation," Read said.
Smaller, smarter trials
From his office at the ICR behind the Marsden hospital in Sutton, Workman has an unusual vantage point across the cancer landscape. With a staff of 160, his team is as large as the oncology departments of some Big Pharma companies and in the past six years has discovered 16 innovative cancer drugs.
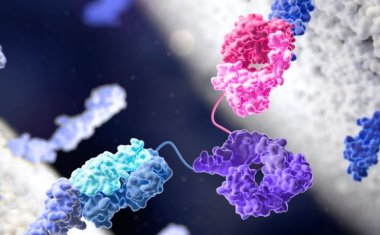
Thanks to rapid advances in genetics, scientists now have a fundamental understanding of the workings of tumour cells that did not exist in the days when toxic chemotherapy was the only tool in the medicine chest.
However, the lion's share of the $1 billion or more it takes to bring a new drug to market is not chewed up by scientists working in the lab but by the cost of running clinical trials. It is the high failure rate of these studies that pushes up the price of those few drugs that do succeed.
Still, there is light at the end of the tunnel. The ability to target modern cancer treatments to the genetic profile of individual patients means trials can now be designed with far fewer patients, reducing costs dramatically.
Workman predicts that in five years the average success rate for a cancer drug starting out in early-stage clinical development will be 50%, up from 5% now.
"It is no longer a lottery," he says.
"Trials in future will be smaller, quicker and cheaper. The failure rate will go down and the economic model will rebalance. That means the R&D costs that companies need to recoup when they sell a new drug will come down and those savings should be passed on to the patients."
There are already encouraging signs. Roche's new melanoma drug Zelboraf, for example, which is designed for patients with one type of abnormal gene, was approved in 2011 less than five years after the start of its first clinical trials - far shorter than the timescale for most drugs.
Even so, modern cancer drugs are never likely to be affordable to the poor of Asia, Africa and Latin America under the current patent-protected system - one reason why MSF's Childs says governments need to investigate new models for rewarding innovation, possibly via a system of upfront payments.
Back at the ICR, Workman's colleague Johann de Bono, who led much of the clinical research on Zytiga, says it is clear something in the current system has to give:
"I'm a Christian, so human life to me is very valuable. But how do you value a human life? It's very difficult."